Side Effect: Mucositis
What is Mucositis?
Mucositis is breakdown of mucosal tissues as a result of cells dying faster than they can regenerate. It is an often painful side effect caused by several types of cancer therapy, including:
- Chemotherapy
- Radiation to the head, neck, gastrointestinal tract, or rectum
- Combination chemotherapy + radiation
- All types of bone marrow transplant (including allogeneic, autologous, and syngeneic)
Mucositis may cause difficulty eating due to pain when chewing or swallowing. Some patients require pain medications, such as opiates. If mucositis prevents someone from eating or drinking, on occasion the person may need to be hospitalized for hydration or intravenous feeding. Because mucositis results from a breakdown in the mucosal barrier, bacterial infections may be more common.
What does Mucositis look like?
Mucositis, when isolated to the mouth, also known as stomatitis, appears as red or ulcerated sores. Based upon the severity of the ulcer, it can be assigned a grade.
Grade I: presence of ulcers that are not painful or are only midly painful
Grade II: presence of moderately painful ulcers but ability to eat and drink is not affected
Grade III: severely painful ulcers affecting ability to eat and drink
Grade IV: severely painful ulcers that are deemed life-threatening if not treated urgently
When mucositis affects the gastrointestinal tract (GI tract), it may lead to nausea, vomiting, bloating, cramping, diarrhea, and abdominal pain.
Mucositis
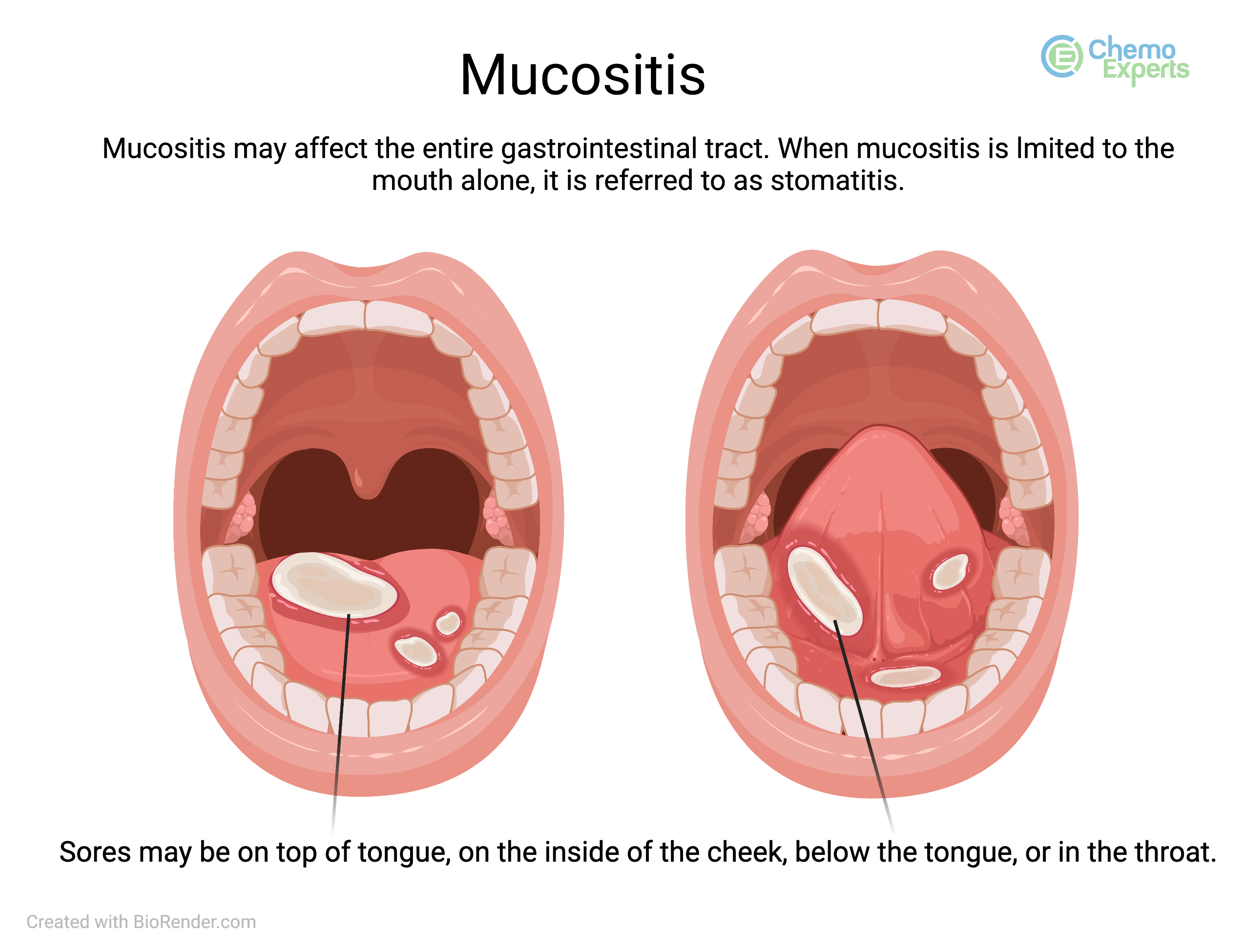
Click to enlarge
This picture of mucosits shows ulceration on and below the tongue. Ulcers may also appear on the inside of the cheeks, on the upper or lower palate, or in the throat.
Who gets Mucositis?
The risk of developing mucositis depends upon several factors, most importantly the specific chemotherapy and/or radiation treatments that you are receiving. For instance, chemotherapy drugs such as fluorouracil (5-FU), methotrexate, etoposide, and melphalan carry a higher risk of mucositis than other chemotherapy agents, but the development of mucositis is not limited to these agents alone. Other risk factors for developing mucositis can include:
- Smoking
- Poor oral hygine
- Younger age
- Female
- Poor nutrition
- Low white blood cell counts (Neutropenia)
How to prevent Mucositis
Basic oral care (BOC)
- Basic oral care throughout treatment is essential to preventing problems before they arise. Basic oral care involves mechanical cleaning such as brushing and flossing, but also includes alcohol-free mouth washes and anti-bacterial rinses.
- It is a good idea to schedule an appointment with your dentist before you start treatment.
- A check-up and cleaning could help to prevent a bacterial infection from developing during treatment, which in turn, may ultimately prevent you from needing to go to the hospital to receive intravenous antibiotics
Prevention options for mucositis depend up the certain medication being used that may be causing this side effect. Some prevention options work for some chemotherapy agents, while having little to no affect on others.
Ice Chips
Sucking on ice chips while receiving an infusion of certain chemotherapy medications (eg. melphalan) may prevent mucositis or lessen its severity. This does not work with all chemotherapy because certain drugs circulate in the blood stream (swim around) longer than others before they are eliminated from the body. To prevent mucositis from these medications, one would need to suck on ice chips for a longer period of time and this may actually cause more harm than good. Ask your doctor, nurse, or pharmacist if sucking on ice chips is recommended with the type of chemotherapy you are receiving.
Dexamethasone
Steroid mouthwashes, such as dexamethasone, may help to prevent mucositis caused specifically by the drug everolimus (Afinitor®). Dexamethasone helps decrease the inflammation of the tissues of the mouth that is caused by everolimus.
Palifermin (Kepivance®)
Palifermin is a medication that can be used to prevent mucositis during autologous stem cell transplant. It works by causing increased production of cells of the mouth, tongue, and throat to replace those cells that were damaged by chemotherapy.
Leucovorin
Leucovorin is given after high-dose methotrexate to reverse the toxic effects of methotrexate and "rescue" non-cancer cells from its effects. By reversing the effects, it helps decrease the risk of side effects of methotrexate such as mucositis.
Supersaturated calcium/phosphate oral rinses
Oral solutions that contain a mixture of calcuim and phosphate (Caphosol® and SalivaMAX®) may be utilized in certain situations, like autologous and allogeneic bone marrow transplant, to protect the tissues of the mouth and help prevent or lessen the severity of mucositis.
How to treat Mucositis
Modify Diet
There are certain types of food and drinks that you should avoid if you are experiencing mucositis as these can either make the ulcers worse or more painful. Some things to avoid include:
- Alcohol (including alcohol containing mouthwashes)
- Spicy foods
- Sharp and rough foods (e.g. potato chips, popcorn, crackers)
- Acidic foods and drinks (e.g. carbonated beverages, juices, fruits, tomato sauce)
- High temperature foods or drinks (e.g. hot coffee, soup, hot tea)
Salt and Soda mouth wash
Mixtures of equal parts of salt and baking soda can be swished around the mouth and spit out several times per day to help relieve some discomfort from mucositis. This mixture helps to soothe minor or moderaly painful ulcers such as those seen in Grade 1 or Grade 2 mucositis.
Lidocaine mouth wash
Lidocaine is a numbing agent that when swished in the mouth can help dull the pain of mouth ulcers. Lidocaine may be given as a rinse by itself or with a combination of other medications such as diphendydramine (Benadryl®), nystatin, hydrocortisone, and/or antacids (e.g. Maalox®), which is sometimes referred to as "magic mouthwash."
Gelclair
Gelclair is a gel-like substance that coats the end of the exposed nerve areas in your mouth, which has been shown to decrease pain. It is a temporary effect. Gelclair has a black licorice taste. If you dislike the taste of black licorice, you may want to ensure that you can tolerate this before puting the full dose in your mouth.
Glucarpidase (Voraxaze®)
For patients recieving high-dose methotrexate, it is very important that methotrexate is cleared from the body in a certain amount of time. If blood methotrexate levels are significantly higher than they should be, your doctor may administer glucarpidase to help the body eliminate methotrexate and lower the risks of side effects which can include severe mucositis
Uridine Triacetate (Vistogard®)
If there happens to be an accidental overdose of fluorouracil (5-FU) or capecitabine (Xeloda®), or if you are a poor metabolizer (cannot elimiate the chemotherapy in a predicatble amount of time), mucositis can occur. Uridine triacitate helps block the effects of 5-FU and capecitabine to lessen the risks of severe side effects like mucositis.
Pain medications:
Mucositis can be so severe that it prevents you from eating and drinking. In these cases, some patients are admitted to the hospital for IV pain medications and other supportive care measures, such as tube feeding or intravenous nutrition, known as TPN (total parenteral nutrition).
Created: February 10, 2024
Updated: February 21, 2024